Location/ Distribution:
May be global or localized to an area
Consistency/ Echogenicity of the fluid:
In majority of cases, echo-free fluid is noted
Sometimes echogenic strands may be seen especially if the effusion is chronic
Echocardiographic features of cardiac tamponade:
· Prolonged and widespread RV diastolic collapse
· A fall by > 40% in early diastolic trans-mitral velocity in inspiration
· Dilated IVC (>2cm) with an inspiratory collapse of <50%
· Dominant systolic SVC flow
Pitfalls in diagnosing tamponade:
- Diastolic collapse of the RA or the RVOT is an oversensitive sign. Can occur
even with small effusions
- The slight diastolic "notching" of the RV wall which is common
in pericardial effusion is not suggestive of tamponade
Rarely in cases of tamponade, RV diastolic collapse may not be clearly seen
(eg: if the RV free wall is stiff or in presence of pulmonary hypertension).
Role of echocardiography in pericardiocentesis:
Prior to pericardiocentesis an echocardiogram must be done to confirm
· The site of aspiration (sub-costal / apical)
· Safety of the procedure: at least ³ 2cm of fluid along the intended needle
track required to allow safe aspiration
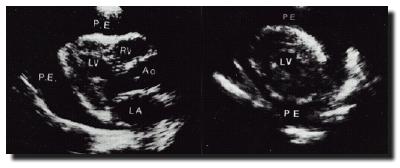
Points to note during scanning:
Set scale of parasternal long axis image small enough to visualize posterior
to the left ventricle. ( A left sided pleural effusion may also be noted if
present)
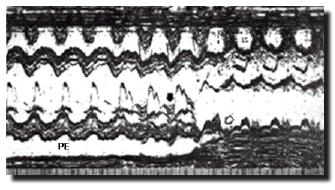
When M mode placed through the RV in the parasternal long axis view, mid-diastolic
"notching" may be noted even with small pericardial effusion. This
should not be confused with diastolic RV collapse.
Sub-costal views are especially useful to visualize the right sided chambers
Structures that may simulate an effusion:
1. Pericardial/ Epicardial fat
may appear similar to a haemopericardium/ pyopericardium
However, unlike in a true pericardial effusion
- constant echoes noted
- no changes with patient position
- no RV notching or signs of Tamponade
2. Left sided Pleural effusion
The differentiating features of a pericardial effusion include
- Pericardial Fluid remains anterior to the descending aorta
- It does not usually extend behind the left atrium
- Usually bobbing of the heart noted
- Signs of tamponade may be present
- Sub-costal views may show fluid between the heart and the diaphragm
- The fluid depth rarely exceeds 4 cm
An echogenic line usually noted separating the two effusions and indicating the interface.